Understanding Heart Failure: Causes, Symptoms, Treatment, and Prevention
Introduction:
Heart failure is a complex medical condition that affects millions of people worldwide. It's a chronic, progressive condition where the heart muscle is unable to pump enough blood to meet the body's needs. Despite advancements in medical science, heart failure remains a significant cause of morbidity and mortality globally. In this comprehensive guide, we'll delve into the intricacies of heart failure, including its causes, symptoms, treatment options, and preventive measures.
Understanding Heart Failure:
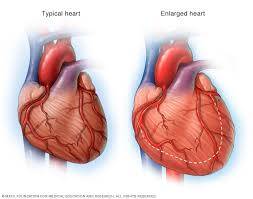
Heart failure occurs when the heart's pumping action becomes weakened or damaged, leading to inadequate blood circulation throughout the body. This condition can affect either the left side, the right side, or both sides of the heart. When the left side fails, it's called left-sided heart failure, and when the right side fails, it's called right-sided heart failure. Both types can occur simultaneously, resulting in congestive heart failure.
Causes of Heart Failure:
1. Coronary Artery Disease (CAD): CAD is the most common cause of heart failure. It occurs when the arteries that supply blood to the heart become narrowed or blocked due to the buildup of plaque (atherosclerosis).
2. Hypertension (High Blood Pressure): Prolonged high blood pressure puts strain on the heart, causing it to thicken and stiffen over time. This can eventually lead to heart failure.
3. Cardiomyopathy: This is a group of diseases that affect the heart muscle, making it harder for the heart to pump blood effectively. Dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy are the three main types.
4. Heart Valve Disorders: Malfunctioning heart valves can disrupt the flow of blood through the heart, leading to heart failure. Common valve disorders include aortic stenosis, mitral regurgitation, and mitral valve prolapse.
5. Myocarditis: Myocarditis is inflammation of the heart muscle, often due to a viral infection. Severe cases can weaken the heart and lead to heart failure.
Symptoms of Heart Failure:
The symptoms of heart failure can vary depending on the severity of the condition and which part of the heart is affected. Common symptoms include:
1. Shortness of breath (dyspnea) during physical exertion or at rest.
2. Fatigue and weakness.
3. Swelling in the legs, ankles, feet, or abdomen (edema).
4. Rapid or irregular heartbeat (palpitations).
5. Persistent coughing or wheezing, especially when lying down.
6. Sudden weight gain due to fluid retention.
7. Reduced ability to exercise.
8. Difficulty concentrating or decreased alertness.
It's essential to note that not everyone with heart failure will experience all of these symptoms, and some individuals may not experience any symptoms at all until the condition becomes advanced.
Diagnosis of Heart Failure:
Diagnosing heart failure typically involves a combination of medical history review, physical examination, and diagnostic tests. These may include:
1. Blood tests: To check for elevated levels of certain proteins that indicate heart muscle damage (e.g., BNP, NT-proBNP).
2. Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart and can help identify abnormalities in heart rhythm or structure.
3. Echocardiogram: An ultrasound of the heart that provides detailed images of its structure and function, including the pumping capacity (ejection fraction).
4. Chest X-ray: To assess the size and shape of the heart and check for signs of fluid buildup in the lungs.
5. Cardiac MRI or CT scan: These imaging tests can provide more detailed information about the heart's structure and function, helping to identify the underlying cause of heart failure.
Treatment Options for Heart Failure:
The goals of treating heart failure are to relieve symptoms, improve quality of life, and slow disease progression. Treatment strategies may include:
1. Lifestyle modifications: Adopting a heart-healthy lifestyle can help manage heart failure symptoms and improve overall health. This may involve maintaining a balanced diet low in sodium and saturated fats, exercising regularly, quitting smoking, limiting alcohol consumption, and managing stress.
2. Medications: Several medications are used to treat heart failure, including:
- ACE inhibitors, ARBs, and angiotensin receptor-neprilysin inhibitors (ARNIs) to relax blood vessels and lower blood pressure.
- Beta-blockers to reduce heart rate and workload on the heart.
- Diuretics (water pills) to reduce fluid buildup and relieve symptoms of congestion.
- Aldosterone antagonists to help reduce fluid retention and improve heart function.
- Digoxin to strengthen heart contractions and regulate heart rhythm.
3. Devices: In some cases, implantable devices may be recommended to help manage heart failure, including:
- Pacemakers to help regulate abnormal heart rhythms.
- Implantable cardioverter-defibrillators (ICDs) to monitor heart rhythm and deliver electrical shocks if life-threatening arrhythmias occur.
- Cardiac resynchronization therapy (CRT) devices to improve synchronization of the heart's chambers and enhance pumping efficiency.
4. Surgical procedures: In severe cases of heart failure, surgery may be necessary to improve heart function or treat underlying conditions. These may include:
- Coronary artery bypass grafting (CABG) to bypass blocked coronary arteries and restore blood flow to the heart.
- Heart valve repair or replacement to correct malfunctioning heart valves.
- Heart transplant for end-stage heart failure when other treatments are no longer effective.
5. Palliative care and hospice: For individuals with advanced heart failure, palliative care and hospice services can provide relief from symptoms, improve quality of life, and offer emotional and spiritual support for patients and their families.
Preventing Heart Failure:
While some risk factors for heart failure, such as age and family history, cannot be changed, there are several steps individuals can take to reduce their risk:
1. Maintain a healthy lifestyle: Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Limit intake of sodium, saturated fats, and added sugars. Exercise regularly and maintain a healthy weight.
2. Manage underlying conditions: Control high blood pressure, diabetes, and high cholesterol through medication, lifestyle modifications, and regular medical follow-up.
3. Avoid smoking and limit alcohol consumption: Smoking damages blood vessels and increases the risk of heart disease, while excessive alcohol consumption can weaken the heart muscle and contribute to heart failure.
4. Get regular check-ups: See your healthcare provider regularly for preventive care and screenings to monitor your heart health and detect any early signs of heart failure.
5. Follow treatment plans: If you have been diagnosed with conditions that increase your risk of heart failure, such as coronary artery disease or hypertension, follow your healthcare provider's recommendations for medications, lifestyle modifications, and monitoring.
Conclusion:
Heart failure is a serious and potentially life-threatening condition that requires comprehensive medical management and ongoing support. By understanding the causes, symptoms, treatment options, and preventive measures for heart failure, individuals can take proactive steps to manage their heart health and reduce their risk of developing this debilitating condition. Early diagnosis and intervention are crucial for improving outcomes and quality of life for people living with heart failure.



No comments yet
Be the first to share your thoughts!