Crohn's Disease: Symptoms, Causes, Diagnosis, and Treatment Options
Introduction to Crohn's Disease
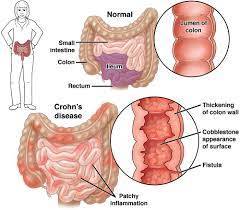
Crohn's Disease, a chronic inflammatory condition of the gastrointestinal (GI) tract, affects millions of people worldwide. It is one of the two main forms of inflammatory bowel disease (IBD), the other being ulcerative colitis. Crohn's Disease can impact any part of the digestive tract, from the mouth to the anus, but it most commonly affects the end of the small intestine (ileum) and the beginning of the large intestine (colon).
This article will delve into the intricate details of Crohn's Disease, including its symptoms, causes, diagnosis, and available treatment options. Understanding this condition is crucial for patients, caregivers, and healthcare professionals alike, as it can significantly impact the quality of life and necessitate long-term management strategies.
Understanding the Symptoms of Crohn's Disease
Crohn's Disease presents a wide range of symptoms, which can vary in severity and manifestation from person to person. Some of the most common symptoms include:
1. Abdominal Pain and Cramping: Persistent and often severe abdominal pain and cramping are hallmark symptoms of Crohn's Disease. These pains may occur even when the individual is not eating and can range from mild to debilitating.
2. Diarrhea: Chronic diarrhea is a prevalent symptom of Crohn's Disease, often accompanied by urgency and a feeling of incomplete evacuation. In some cases, diarrhea may be bloody.
3. Fatigue: Many individuals with Crohn's Disease experience fatigue, which can be debilitating and impact daily functioning.
4. Weight Loss: Unintentional weight loss is common in individuals with Crohn's Disease, often due to decreased appetite, malabsorption of nutrients, and increased metabolic demands from inflammation.
5. Rectal Bleeding: Rectal bleeding can occur in Crohn's Disease, particularly when the colon or rectum is involved. The presence of blood in the stool should always be evaluated by a healthcare professional.
6. Fever: Fever is a systemic symptom that may accompany Crohn's Disease during periods of active inflammation or infection.
7. Other Symptoms: Additional symptoms may include nausea, vomiting, reduced appetite, joint pain, skin problems, and eye inflammation.
It is important to note that Crohn's Disease can also lead to complications outside the digestive tract, such as arthritis, skin disorders, liver disease, kidney stones, and osteoporosis.
Understanding the Causes of Crohn's Disease
The exact cause of Crohn's Disease remains unknown, but it is believed to involve a combination of genetic, environmental, immunological, and microbial factors. Several theories have been proposed to explain the development of Crohn's Disease:
1. Genetic Factors: There is a strong genetic component to Crohn's Disease, with family history being a significant risk factor. Mutations in certain genes, such as NOD2 and ATG16L1, have been implicated in the development of Crohn's Disease.
2. Environmental Triggers: Environmental factors, such as diet, smoking, infections, and exposure to certain medications, may trigger or exacerbate Crohn's Disease in susceptible individuals.
3. Dysregulated Immune Response: Crohn's Disease is characterized by an abnormal immune response in the GI tract, where the immune system mistakenly attacks harmless bacteria, food particles, and cells lining the digestive tract, leading to inflammation and tissue damage.
4. Alterations in Gut Microbiota: Changes in the composition and function of the gut microbiota, the trillions of microorganisms residing in the digestive tract, have been implicated in the pathogenesis of Crohn's Disease. Disruption of the delicate balance between beneficial and harmful bacteria may contribute to intestinal inflammation and disease progression.
5. Barrier Dysfunction: Dysfunction of the intestinal epithelial barrier, which normally serves to prevent the passage of harmful substances from the gut into the bloodstream, may play a role in the development of Crohn's Disease. Increased intestinal permeability allows bacteria and other antigens to penetrate the intestinal wall, triggering an immune response and inflammation.
While these factors are believed to contribute to the development of Crohn's Disease, the interplay between genetics, environment, and the immune system is complex and not fully understood.
Diagnosing Crohn's Disease
Diagnosing Crohn's Disease can be challenging, as its symptoms overlap with those of other gastrointestinal conditions. A comprehensive evaluation is necessary to establish a diagnosis and differentiate Crohn's Disease from conditions such as ulcerative colitis, irritable bowel syndrome (IBS), celiac disease, and gastrointestinal infections. The diagnostic process typically involves the following steps:
1. Medical History: The healthcare provider will take a detailed medical history, including symptoms, family history, medication use, and past medical conditions.
2. Physical Examination: A physical examination may reveal abdominal tenderness, palpable masses, and signs of malnutrition or dehydration.
3. Laboratory Tests: Blood tests may be performed to assess for signs of inflammation (e.g., elevated C-reactive protein and erythrocyte sedimentation rate), anemia, electrolyte imbalances, and nutritional deficiencies.
4. Stool Studies: Stool samples may be analyzed for the presence of blood, infectious organisms, and markers of inflammation (e.g., calprotectin).
5. Imaging Studies: Imaging studies, such as X-rays, ultrasound, computed tomography (CT) scans, and magnetic resonance imaging (MRI), may be used to visualize the digestive tract and detect abnormalities such as inflammation, strictures, fistulas, and abscesses.
6. Endoscopic Procedures: Endoscopic procedures, including colonoscopy and upper endoscopy (esophagogastroduodenoscopy), allow for direct visualization of the GI tract and the collection of tissue samples (biopsies) for microscopic examination. These procedures are essential for confirming the diagnosis of Crohn's Disease and assessing disease severity and extent.
Once a diagnosis of Crohn's Disease is established, further evaluation may be needed to assess for complications and determine the most appropriate treatment approach.
Treatment Options for Crohn's Disease
The management of Crohn's Disease aims to alleviate symptoms, induce and maintain remission, prevent complications, and improve the patient's quality of life. Treatment strategies may vary depending on the severity and location of the disease, as well as individual patient factors such as age, overall health, and treatment preferences. The main treatment modalities for Crohn's Disease include:
1. Medications: Various medications may be used to control inflammation, suppress the immune system, alleviate symptoms, and promote healing of the intestinal mucosa. Commonly prescribed medications for Crohn's Disease include:
- Aminosalicylates (e.g., mesalamine): These drugs help reduce inflammation in the lining of the GI tract and are often used to treat mild to moderate Crohn's Disease.
- Corticosteroids (e.g., prednisone, budesonide): These powerful anti-inflammatory drugs are used to induce remission in moderate to severe Crohn's Disease but are not suitable for long-term use due to their potential side effects.
- Immunomodulators (e.g., azathioprine, 6-mercaptopurine, methotrexate): These drugs work by suppressing the immune system and are used to maintain remission and reduce the need for corticosteroids.
- Biologic therapies (e.g., anti-TNF agents, vedolizumab, ustekinumab): Biologic drugs target
specific molecules involved in the inflammatory process and are highly effective in inducing and maintaining remission in moderate to severe Crohn's Disease.
2. Nutritional Therapy: Exclusive enteral nutrition (EEN), which involves consuming a liquid formula diet for a period of several weeks, has been shown to induce remission in some individuals with Crohn's Disease, particularly children and adolescents. Nutritional supplements may also be used to correct nutrient deficiencies and support overall health.
3. Surgery: Surgery may be necessary for individuals with complications of Crohn's Disease, such as strictures, fistulas, abscesses, and bowel obstructions, or for those who do not respond to medical therapy. Surgical procedures may involve removing the affected portion of the intestine (resection), repairing fistulas or abscesses, or creating a temporary or permanent stoma (ileostomy or colostomy).
4. Lifestyle Modifications: Adopting a healthy lifestyle can help manage symptoms and improve overall well-being in individuals with Crohn's Disease. This includes maintaining a nutritious diet, staying hydrated, avoiding trigger foods, managing stress, getting regular exercise, getting enough sleep, and avoiding smoking and excessive alcohol consumption.
5. Supportive Therapies: Supportive therapies such as counseling, support groups, and complementary and alternative medicine modalities (e.g., acupuncture, herbal supplements) may help individuals cope with the physical and emotional challenges of living with Crohn's Disease.
It is important for individuals with Crohn's Disease to work closely with their healthcare team to develop a personalized treatment plan tailored to their specific needs and preferences. Regular monitoring and follow-up are essential to assess treatment response, monitor for potential side effects, and adjust therapy as needed.
Conclusion
Crohn's Disease is a complex and challenging condition that can significantly impact the lives of affected individuals. While the exact cause of Crohn's Disease remains unclear, it is believed to involve a combination of genetic, environmental, immunological, and microbial factors. Early diagnosis and comprehensive management are essential for optimizing outcomes and improving the quality of life for individuals with Crohn's Disease.
By understanding the symptoms, causes, diagnosis, and treatment options for Crohn's Disease, patients, caregivers, and healthcare professionals can work together to effectively manage this chronic condition and minimize its impact on daily life. With ongoing research and advances in treatment, there is hope for better outcomes and improved quality of life for individuals living with Crohn's Disease.



No comments yet
Be the first to share your thoughts!