Understanding Ulcerative Colitis
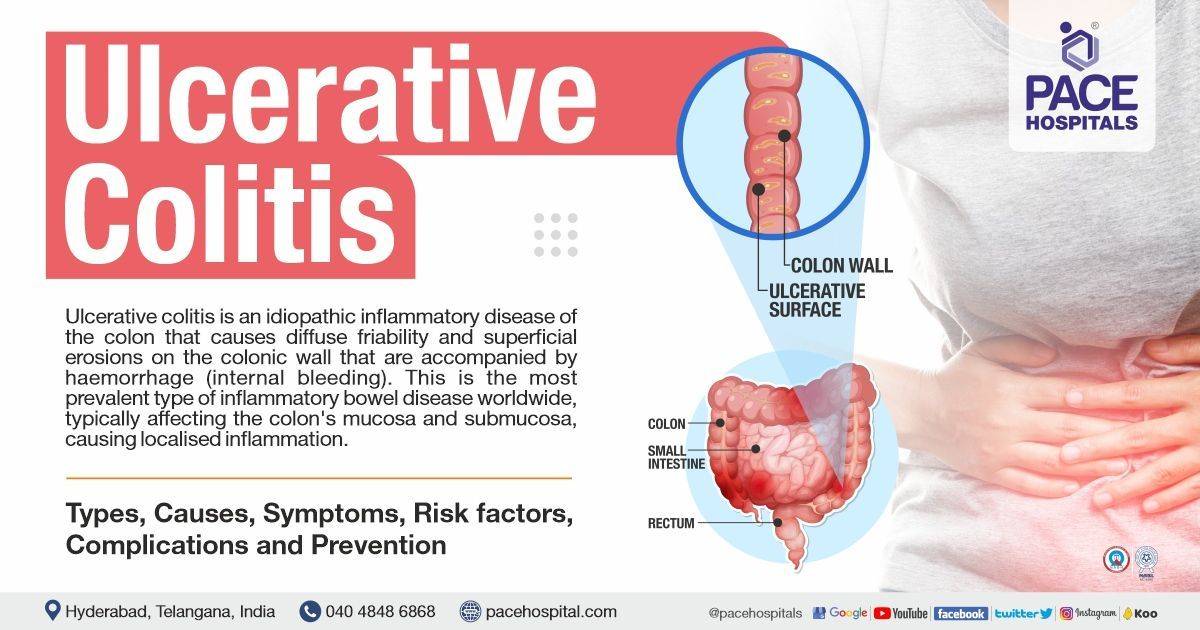
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) characterized by inflammation and ulcers in the lining of the colon and rectum. It is a condition that affects millions of people worldwide, with symptoms ranging from mild to severe and often impacting various aspects of daily life. In this comprehensive guide, we will delve into the causes, symptoms, diagnosis, treatment options, and management strategies for ulcerative colitis.
### Understanding Ulcerative Colitis
#### What Causes Ulcerative Colitis?
The exact cause of ulcerative colitis remains unknown, but it is believed to involve a complex interplay of genetic, environmental, and immune factors. Family history of IBD, genetics, abnormal immune system response, and environmental triggers such as diet, stress, and certain medications are thought to contribute to the development of UC. However, the precise mechanisms underlying the condition are still being researched.
#### Symptoms of Ulcerative Colitis
Symptoms of ulcerative colitis can vary widely depending on the severity and location of inflammation within the colon and rectum. Common symptoms include:
1. **Diarrhea:** Frequent, urgent bowel movements with blood or pus.
2. **Abdominal Pain:** Cramping or abdominal discomfort, often relieved by bowel movements.
3. **Rectal Bleeding:** Blood in the stool, ranging from mild to severe.
4. **Urgency:** Sudden and urgent need to have a bowel movement.
5. **Fatigue:** Feeling tired or lethargic, often due to anemia from blood loss.
6. **Weight Loss:** Loss of appetite and unintentional weight loss may occur, especially during flare-ups.
7. **Fever:** Low-grade fever may accompany inflammation.
It is essential to note that symptoms can fluctuate over time, with periods of remission (when symptoms are absent) and flare-ups (when symptoms worsen).
#### Diagnosis of Ulcerative Colitis
Diagnosing ulcerative colitis typically involves a combination of medical history, physical examination, and various diagnostic tests. These may include:
1. **Blood Tests:** To check for signs of inflammation, anemia, and to rule out other possible causes of symptoms.
2. **Stool Sample Analysis:** To detect the presence of blood, infection, or other abnormalities in the stool.
3. **Colonoscopy:** A procedure in which a flexible tube with a camera is inserted into the rectum and colon to visualize the lining and obtain tissue samples (biopsies) for examination under a microscope.
4. **Imaging Tests:** Such as CT scans or MRIs, to assess the extent and severity of inflammation and complications.
#### Types and Classification of Ulcerative Colitis
Ulcerative colitis can be classified based on the location and severity of inflammation within the colon and rectum. The main types include:
1. **Ulcerative Proctitis:** Inflammation limited to the rectum, which may cause rectal bleeding and discomfort.
2. **Proctosigmoiditis:** Inflammation involving the rectum and sigmoid colon (lower part of the colon), characterized by symptoms such as bloody diarrhea, urgency, and tenesmus (the feeling of incomplete bowel movements).
3. **Left-sided Colitis:** Inflammation extending from the rectum up to the splenic flexure (where the colon bends near the spleen), leading to symptoms such as abdominal pain, diarrhea, and rectal bleeding.
4. **Pancolitis:** Inflammation affecting the entire colon, resulting in severe symptoms including diarrhea, abdominal pain, weight loss, and fatigue.
#### Treatment Options for Ulcerative Colitis
The goals of treatment for ulcerative colitis are to induce and maintain remission, reduce inflammation, alleviate symptoms, and improve the quality of life for patients. Treatment approaches may vary depending on the severity and extent of the disease, as well as individual factors such as age, overall health, and treatment preferences. Common treatment options include:
1. **Medications:**
- **Aminosalicylates:** Anti-inflammatory drugs such as mesalamine, sulfasalazine, and balsalazide, which are often used as first-line therapy for mild to moderate UC.
- **Corticosteroids:** Such as prednisone or budesonide, may be prescribed to reduce inflammation during flare-ups but are not suitable for long-term use due to potential side effects.
- **Immunomodulators:** Drugs like azathioprine, 6-mercaptopurine, or methotrexate may be used to suppress the immune system and maintain remission in moderate to severe cases.
- **Biologic Therapies:** Targeted therapies such as anti-TNF agents (infliximab, adalimumab, golimumab), vedolizumab, or ustekinumab, which block specific pathways involved in inflammation, are often reserved for patients who do not respond to conventional treatments.
2. **Dietary and Lifestyle Modifications:**
- **Low-Residue Diet:** Limiting high-fiber foods that may exacerbate symptoms during flare-ups.
- **Nutritional Supplements:** Ensuring adequate intake of nutrients, especially during periods of reduced appetite or malabsorption.
- **Stress Management:** Techniques such as relaxation exercises, meditation, and counseling may help reduce stress and improve symptom control.
3. **Surgery:** In cases of severe, refractory UC or complications such as toxic megacolon, perforation, or cancer, surgical removal of the colon (colectomy) may be necessary. This may involve creating an ileal pouch-anal anastomosis (IPAA or J-pouch) or a permanent ileostomy, where the end of the small intestine is connected to an opening in the abdominal wall (stoma) to allow for the passage of stool.
#### Management of Ulcerative Colitis
In addition to medical treatment, effective management of ulcerative colitis involves regular monitoring, lifestyle modifications, and ongoing support. Here are some key strategies:
1. **Regular Follow-up:** Patients with UC require regular check-ups with their healthcare providers to monitor disease activity, adjust treatment as needed, and address any concerns or complications.
2. **Medication Adherence:** It is essential for patients to take their prescribed medications as directed by their healthcare providers, even during periods of remission, to prevent relapses and maintain long-term control of the disease.
3. **Monitoring for Complications:** Regular screening for complications such as colorectal cancer, osteoporosis, and nutritional deficiencies is crucial for early detection and intervention.
4. **Healthy Lifestyle:** Adopting a healthy lifestyle, including a balanced diet, regular exercise, adequate hydration, and avoidance of smoking and excessive alcohol consumption, can help support overall well-being and improve disease outcomes.
5. **Supportive Care:** Joining support groups, participating in patient education programs, and seeking emotional support from friends, family, or mental health professionals can help patients cope with the physical and emotional challenges of living with ulcerative colitis.
### Conclusion
Ulcerative colitis is a chronic inflammatory bowel disease that can have a significant impact on the lives of affected individuals. While the exact cause remains unclear, advancements in research have led to improved understanding of the disease mechanisms and treatment options. With a multidisciplinary approach involving medical therapy, dietary and lifestyle modifications, and ongoing support, many patients with UC can achieve long-term remission and maintain a
good quality of life. However, it is essential for patients to work closely with their healthcare providers, adhere to treatment regimens, and actively participate in their care to effectively manage the disease and minimize complications.



No comments yet
Be the first to share your thoughts!