Understanding Coronary Artery Disease: Causes, Symptoms, Treatment, and Prevention
Introduction:
Coronary artery disease (CAD) remains one of the leading causes of morbidity and mortality worldwide, representing a significant public health challenge. Also known as ischemic heart disease, CAD occurs when the blood vessels supplying the heart muscle become narrowed or blocked, leading to reduced blood flow to the heart. This article aims to provide a comprehensive overview of coronary artery disease, including its causes, symptoms, treatment options, and preventive measures.
Section 1: Understanding Coronary Artery Disease
1.1 Definition and Anatomy:
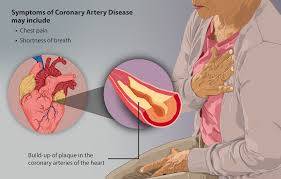
Coronary artery disease involves the gradual buildup of plaque—a combination of cholesterol, fat, and other substances—within the coronary arteries. These arteries are responsible for supplying oxygen-rich blood to the heart muscle, enabling it to function effectively. When plaque accumulates within these arteries, it restricts blood flow, leading to various cardiovascular complications.
1.2 Pathophysiology:
The development of coronary artery disease typically begins with endothelial dysfunction, where the inner lining of the arteries becomes damaged. This damage allows substances like low-density lipoprotein (LDL) cholesterol to infiltrate the arterial walls, triggering an inflammatory response. Over time, this process leads to the formation of atherosclerotic plaques, which can gradually narrow or completely block the affected arteries.
1.3 Risk Factors:
Several factors contribute to the development of coronary artery disease, including:
- High blood pressure (hypertension)
- High cholesterol levels (hypercholesterolemia)
- Smoking
- Diabetes
- Obesity
- Sedentary lifestyle
- Family history of heart disease
- Age (risk increases with age)
Understanding these risk factors is crucial for identifying individuals who may be at higher risk of developing CAD and implementing preventive measures accordingly.
Section 2: Symptoms and Diagnosis
2.1 Symptoms:
The symptoms of coronary artery disease can vary depending on the severity of the condition and the extent of arterial blockage. Common symptoms include:
- Chest pain or discomfort (angina), often described as pressure, tightness, or a squeezing sensation in the chest
- Shortness of breath
- Fatigue
- Nausea
- Dizziness
- Sweating
It's essential to recognize these symptoms promptly and seek medical attention, as untreated CAD can lead to serious complications such as heart attack or sudden cardiac arrest.
2.2 Diagnosis:
Diagnosing coronary artery disease typically involves a combination of medical history evaluation, physical examination, and diagnostic tests, including:
- Electrocardiogram (ECG/EKG): This test records the electrical activity of the heart and can detect abnormal rhythms or signs of myocardial ischemia.
- Stress tests: These tests evaluate the heart's function during physical exertion and can help identify areas of reduced blood flow to the heart muscle.
- Coronary angiography: This invasive procedure involves injecting a contrast dye into the coronary arteries to visualize any blockages or narrowing using X-ray imaging.
- Cardiac CT or MRI: These imaging techniques can provide detailed images of the heart and coronary arteries, helping to assess the extent of arterial blockage.
Section 3: Treatment Options
3.1 Lifestyle Modifications:
For individuals diagnosed with coronary artery disease, making lifestyle changes is a crucial component of treatment. These changes may include:
- Adopting a heart-healthy diet low in saturated fat, cholesterol, and sodium
- Engaging in regular physical activity
- Quitting smoking
- Maintaining a healthy weight
- Managing stress effectively
These lifestyle modifications can help improve cardiovascular health and reduce the progression of coronary artery disease.
3.2 Medications:
Several medications are commonly prescribed to manage coronary artery disease and its associated risk factors, including:
- Statins: These drugs help lower cholesterol levels and reduce the risk of plaque buildup within the arteries.
- Antiplatelet agents: Medications such as aspirin or clopidogrel can help prevent blood clots from forming within the coronary arteries, reducing the risk of heart attack.
- Beta-blockers: These drugs can help lower blood pressure, reduce heart rate, and decrease the heart's workload, thereby relieving symptoms of angina.
- ACE inhibitors or angiotensin II receptor blockers (ARBs): These medications are used to treat hypertension and can help improve outcomes in individuals with coronary artery disease.
3.3 Invasive Procedures:
In cases where lifestyle modifications and medications are insufficient to manage coronary artery disease, invasive procedures may be necessary. These procedures include:
- Percutaneous coronary intervention (PCI): Also known as angioplasty, PCI involves using a catheter with a balloon at its tip to widen narrowed or blocked coronary arteries. In some cases, a stent may be placed to help keep the artery open.
- Coronary artery bypass grafting (CABG): This surgical procedure involves rerouting blood flow around a blocked coronary artery using a healthy blood vessel graft, typically taken from the patient's leg or chest wall.
The choice of treatment approach depends on various factors, including the severity and location of arterial blockages, overall health status, and individual patient preferences.
Section 4: Prevention Strategies
4.1 Primary Prevention:
Preventing coronary artery disease begins with addressing modifiable risk factors and adopting a heart-healthy lifestyle. This includes:
- Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins
- Engaging in regular physical activity, aiming for at least 150 minutes of moderate-intensity exercise per week
- Avoiding tobacco products and minimizing alcohol consumption
- Managing chronic conditions such as hypertension, diabetes, and high cholesterol through medication and lifestyle modifications
4.2 Secondary Prevention:
For individuals with known coronary artery disease, secondary prevention strategies are aimed at reducing the risk of recurrent cardiovascular events. These may include:
- Adhering to prescribed medications as directed by a healthcare provider
- Participating in cardiac rehabilitation programs, which offer structured exercise training, education, and psychosocial support
- Undergoing regular medical follow-ups to monitor disease progression and adjust treatment as needed
By implementing these preventive measures, individuals can significantly reduce their risk of developing coronary artery disease or experiencing complications associated with existing disease.
Conclusion:
Coronary artery disease is a complex and multifactorial condition that requires a comprehensive approach to diagnosis, treatment, and prevention. By understanding the underlying mechanisms of the disease, identifying modifiable risk factors, and implementing appropriate lifestyle modifications and medical interventions, individuals can effectively manage coronary artery disease and improve their long-term cardiovascular health. Through ongoing research and public health initiatives, efforts to combat this pervasive condition continue, with the ultimate goal of reducing its global burden and improving outcomes for affected individuals.



No comments yet
Be the first to share your thoughts!