Tuberculosis: Causes, Symptoms, Treatment, and Prevention
Introduction to Tuberculosis
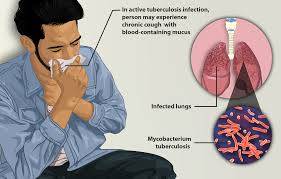
Tuberculosis (TB) is a global health threat caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs but can also target other parts of the body, such as the brain, spine, or kidneys. TB remains one of the top infectious killers worldwide, with an estimated 10 million people falling ill with the disease each year, and approximately 1.5 million succumbing to it.
Despite significant advancements in medicine and public health, TB continues to pose challenges, particularly in regions with limited resources and vulnerable populations. In this comprehensive guide, we delve into the intricacies of tuberculosis, exploring its causes, symptoms, diagnosis, treatment options, and preventive measures.
Understanding the Causes of Tuberculosis
Tuberculosis is an airborne disease, primarily spread through the inhalation of droplets containing Mycobacterium tuberculosis. When an infected person coughs, sneezes, or speaks, tiny droplets containing the bacteria can linger in the air for hours, potentially infecting others who inhale them.
However, not everyone exposed to the bacteria becomes ill. The immune system plays a crucial role in determining whether the infection progresses to active disease. In many cases, the body's immune response is sufficient to control the bacteria, leading to latent tuberculosis infection (LTBI). People with LTBI do not exhibit symptoms and are not contagious, but they are at risk of developing active TB in the future if their immune system weakens.
Several factors can increase the risk of developing active tuberculosis:
1. Weakened Immune System: Individuals with weakened immune systems due to conditions such as HIV/AIDS, diabetes, malnutrition, or certain medications are more susceptible to developing active TB.
2. Close Contact with an Infectious Person: Living or working in close proximity to someone with active TB increases the risk of transmission.
3. Age: Infants, young children, and the elderly are at higher risk of developing TB due to weaker immune responses.
4. Substance Abuse: Substance abuse, particularly intravenous drug use, can weaken the immune system and increase susceptibility to TB.
5. Poverty and Overcrowding: Socioeconomic factors such as poverty, inadequate housing, and overcrowding facilitate the spread of TB, especially in urban slums and refugee camps.
Symptoms of Tuberculosis
The symptoms of tuberculosis can vary depending on whether the infection is active or latent. In latent tuberculosis infection, there are typically no symptoms, and the person is not contagious. However, in active TB disease, symptoms may manifest and worsen over time.
Common symptoms of active tuberculosis include:
1. Persistent Cough: A cough that lasts for more than three weeks is a common symptom of TB. The cough may produce sputum or blood.
2. Chest Pain: Chest pain may occur due to inflammation of the lungs or the formation of cavities.
3. Fatigue: Generalized fatigue and weakness are common symptoms of TB.
4. Weight Loss: Unexplained weight loss is often associated with active tuberculosis.
5. Fever and Night Sweats: Low-grade fever and night sweats are characteristic symptoms, particularly in the later stages of the disease.
6. Loss of Appetite: Decreased appetite and nausea may occur, leading to further weight loss.
It's essential to seek medical attention if you experience any of these symptoms, especially if you have risk factors for tuberculosis.
Diagnosing Tuberculosis
Diagnosing tuberculosis requires a combination of clinical evaluation, medical history, imaging tests, and laboratory tests. The following are common diagnostic methods used to identify TB:
1. Tuberculin Skin Test (TST): Also known as the Mantoux tuberculin skin test, TST involves injecting a small amount of purified protein derivative (PPD) into the skin of the forearm. A healthcare provider then evaluates the reaction after 48 to 72 hours. A positive reaction indicates exposure to TB bacteria but does not distinguish between latent infection and active disease.
2. Interferon-Gamma Release Assays (IGRAs): IGRAs measure the release of interferon-gamma by T-cells in response to antigens specific to Mycobacterium tuberculosis. Unlike the TST, IGRAs do not cross-react with the Bacillus Calmette-Guérin (BCG) vaccine, making them useful in populations where BCG vaccination is common.
3. Chest X-ray: A chest X-ray can reveal abnormalities in the lungs suggestive of tuberculosis, such as infiltrates, cavities, or lymph node enlargement. However, it cannot definitively diagnose TB, as other lung conditions can produce similar findings.
4. Sputum Smear Microscopy: This test involves examining sputum samples under a microscope to detect the presence of acid-fast bacilli (AFB), which are characteristic of Mycobacterium tuberculosis. While widely available and inexpensive, sputum smear microscopy has limitations in terms of sensitivity, particularly in patients with low bacterial loads.
5. Nucleic Acid Amplification Tests (NAATs): NAATs detect Mycobacterium tuberculosis DNA in sputum samples with high sensitivity and specificity. These tests, such as the Xpert MTB/RIF assay, can rapidly diagnose TB and detect resistance to the antibiotic rifampicin, a first-line drug for TB treatment.
Treatment of Tuberculosis
Effective treatment is essential for curing tuberculosis, preventing transmission, and reducing the risk of drug resistance. TB treatment typically involves a combination of antibiotics taken over several months. The most commonly used drugs for TB treatment include:
1. Isoniazid (INH): Isoniazid is a first-line antibiotic that targets actively dividing Mycobacterium tuberculosis. It is often used in combination with other drugs for the treatment of both latent and active TB.
2. Rifampicin (RIF): Rifampicin is another first-line drug that is highly effective against TB bacteria. It is often used in combination with INH for the treatment of active TB.
3. Pyrazinamide (PZA): Pyrazinamide is used in the initial phase of TB treatment to rapidly reduce the bacterial load. It is typically administered for the first two months of therapy.
4. Ethambutol (EMB): Ethambutol is included in the initial treatment regimen for TB to prevent the development of drug resistance. It is particularly effective when used in combination with other first-line drugs.
In addition to these first-line drugs, second-line antibiotics may be necessary to treat drug-resistant TB strains. Treatment regimens for drug-resistant TB are more complex and may require prolonged therapy with multiple antibiotics.
It's crucial to complete the entire course of TB treatment, even if symptoms improve before the medication is finished. Failure to complete treatment can lead to treatment failure, relapse, or the development of drug-resistant TB.
Preventing Tuberculosis
Preventing tuberculosis requires a multifaceted approach that includes vaccination, infection control measures, and addressing social determinants of health. Key strategies for TB prevention include:
1. Bacillus Calmette-Guérin (BCG) Vaccination: The BCG vaccine is a live attenuated vaccine derived from Mycobacterium bovis, which provides partial protection against TB, particularly severe forms of the disease in children. While BCG vaccination is widely used in countries with a high burden of TB, its efficacy in preventing pulmonary TB in adults is variable.
2. Infection Control Measures: In healthcare settings, implementing infection control measures such as proper ventilation, respiratory hygiene, and the use of personal protective equipment can reduce the risk of TB transmission among patients and healthcare workers.
3. Screening and Treatment of Latent TB: Identifying and treating individuals with latent TB infection can prevent progression to active disease and reduce the pool of TB cases in the community.
4. Addressing Social Determinants of Health: Addressing underlying social determinants of health, such as poverty, homelessness, and lack of access to healthcare, is essential for controlling TB transmission and improving health outcomes in vulnerable populations.
Conclusion
Tuberculosis remains a significant global health challenge, particularly in low- and middle-income countries and among vulnerable populations. Despite advancements in diagnosis and treatment, TB continues to exact a heavy toll on human lives and healthcare systems worldwide. Efforts to combat TB require a coordinated, multi-sectoral approach that addresses underlying social determinants of health, strengthens healthcare systems, and promotes equitable access to quality care.
By raising awareness, investing in research and innovation, and prioritizing TB control efforts, we can work towards achieving the goal of ending the tuberculosis epidemic and ensuring a healthier future for all.



No comments yet
Be the first to share your thoughts!