Irritable Bowel Syndrome (IBS): Symptoms, Causes, Diagnosis, and Management
Introduction:
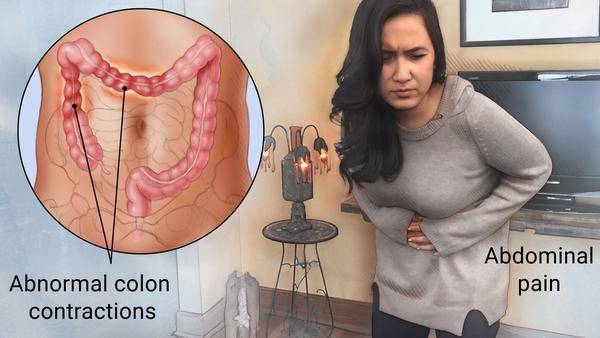
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder that affects millions of people worldwide. Characterized by a combination of symptoms including abdominal pain, bloating, diarrhea, and constipation, IBS can significantly impact an individual's quality of life. Despite its prevalence, the exact cause of IBS remains unclear, and diagnosis can often be challenging. However, advancements in research and treatment options offer hope for better management of this condition. In this comprehensive guide, we will explore the various aspects of IBS, including its symptoms, causes, diagnosis, and management strategies.
Understanding Irritable Bowel Syndrome (IBS):
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder, meaning it affects the functioning of the digestive system without causing structural damage. It is estimated to affect between 10% to 15% of the global population, making it one of the most common gastrointestinal disorders worldwide. IBS can occur at any age, but it is most commonly diagnosed in individuals under the age of 50.
Symptoms of IBS:
The symptoms of IBS can vary widely among individuals and may include:
1. Abdominal pain or discomfort: This is often described as cramping or aching, and it is typically relieved by passing stool.
2. Bloating: Many people with IBS experience bloating, which is a feeling of fullness or tightness in the abdomen.
3. Changes in bowel habits: Individuals with IBS may experience diarrhea, constipation, or alternating episodes of both.
4. Excess gas: Gas and flatulence are common symptoms of IBS.
5. Mucus in the stool: Some people with IBS may notice mucus in their stool.
These symptoms can range from mild to severe and may come and go over time. They can also be triggered or exacerbated by certain foods, stress, hormonal changes, or other factors.
Causes of IBS:
The exact cause of IBS is not fully understood, but several factors may contribute to its development, including:
1. Abnormal gastrointestinal motility: People with IBS may have abnormal contractions of the muscles in the digestive tract, leading to symptoms such as diarrhea or constipation.
2. Intestinal inflammation: Some research suggests that low-grade inflammation in the intestines may play a role in the development of IBS.
3. Altered gut microbiota: The balance of bacteria in the gut, known as the gut microbiota, may be disrupted in individuals with IBS.
4. Food sensitivities: Certain foods and beverages, such as dairy products, gluten, and high-fat foods, may trigger symptoms in some people with IBS.
5. Psychological factors: Stress, anxiety, and depression are common triggers for IBS symptoms in many individuals.
It's important to note that while these factors may contribute to the development of IBS, they do not cause the condition outright. IBS is a complex disorder with multiple underlying mechanisms.
Diagnosis of IBS:
Diagnosing IBS can be challenging because there are no specific tests or biomarkers for the condition. Instead, healthcare providers rely on a combination of medical history, physical examination, and diagnostic tests to rule out other potential causes of symptoms. The Rome criteria, a set of guidelines developed by experts in the field, are often used to diagnose IBS. According to these criteria, a diagnosis of IBS may be considered if an individual experiences recurrent abdominal pain or discomfort at least three days per month for the past three months, along with two or more of the following:
1. Improvement with defecation
2. Onset associated with a change in stool frequency
3. Onset associated with a change in stool form
In some cases, additional tests such as blood tests, stool tests, imaging studies, or endoscopic procedures may be recommended to rule out other conditions that can mimic IBS, such as inflammatory bowel disease (IBD), celiac disease, or colon cancer.
Management of IBS:
While there is no cure for IBS, there are several treatment options available to help manage symptoms and improve quality of life. Treatment strategies for IBS may include:
1. Dietary modifications: Many people with IBS find relief from symptoms by identifying and avoiding trigger foods. Common trigger foods include dairy products, gluten, high-fat foods, caffeine, and artificial sweeteners. Some individuals may also benefit from following a low FODMAP diet, which restricts certain types of carbohydrates that can ferment in the gut and cause symptoms.
2. Lifestyle changes: Stress management techniques such as relaxation exercises, meditation, yoga, and regular physical activity may help reduce IBS symptoms. Getting an adequate amount of sleep and avoiding smoking and excessive alcohol consumption are also important for managing IBS.
3. Medications: Over-the-counter and prescription medications may be recommended to help alleviate specific symptoms of IBS. These may include antispasmodic medications to reduce abdominal cramping, fiber supplements to improve bowel function, laxatives or antidiarrheal medications to regulate bowel movements, and antidepressant medications to help manage pain and improve mood.
4. Psychological therapies: Cognitive-behavioral therapy (CBT), hypnotherapy, and other psychological therapies may be beneficial for individuals with IBS, particularly those who experience significant stress or anxiety related to their symptoms.
5. Alternative therapies: Some people with IBS may find relief from symptoms with acupuncture, probiotics, herbal supplements, or other alternative therapies. However, more research is needed to determine the safety and effectiveness of these treatments for IBS.
It's important for individuals with IBS to work closely with their healthcare providers to develop a personalized treatment plan that addresses their specific symptoms and needs. Regular follow-up appointments may be necessary to monitor symptoms, adjust treatment as needed, and ensure optimal management of the condition.
Conclusion:
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder characterized by symptoms such as abdominal pain, bloating, diarrhea, and constipation. While the exact cause of IBS remains unclear, it is thought to involve a combination of factors including abnormal gastrointestinal motility, intestinal inflammation, altered gut microbiota, food sensitivities, and psychological factors. Diagnosis of IBS can be challenging, but healthcare providers rely on a combination of medical history, physical examination, and diagnostic tests to rule out other potential causes of symptoms. Management of IBS typically involves dietary modifications, lifestyle changes, medications, psychological therapies, and alternative treatments aimed at relieving symptoms and improving quality of life. By working closely with their healthcare providers, individuals with IBS can develop a personalized treatment plan that addresses their specific needs and helps them effectively manage their condition.



No comments yet
Be the first to share your thoughts!