Addison's Disease: Causes, Symptoms, Diagnosis, and Treatment
Introduction to Addison's Disease
Addison's Disease, also known as primary adrenal insufficiency or hypocortisolism, is a rare but potentially life-threatening disorder that affects the adrenal glands. Named after Dr. Thomas Addison, who first described the condition in 1855, Addison's Disease occurs when the adrenal glands fail to produce enough cortisol and often aldosterone, two essential hormones for various bodily functions.
This chronic condition requires lifelong management, as untreated Addison's Disease can lead to serious complications, including adrenal crisis, which is a medical emergency. In this comprehensive guide, we'll delve into the causes, symptoms, diagnosis, and treatment options for Addison's Disease.
Understanding the Adrenal Glands
To comprehend Addison's Disease fully, it's crucial to understand the role of the adrenal glands. These small, triangular-shaped glands are located on top of each kidney. Despite their small size, they play a vital role in regulating several essential functions in the body.
The adrenal glands have two distinct parts: the adrenal cortex and the adrenal medulla. The outer adrenal cortex produces several hormones, including cortisol, aldosterone, and DHEA (dehydroepiandrosterone). Cortisol, often referred to as the "stress hormone," helps regulate metabolism, blood sugar levels, and the body's response to stress. Aldosterone regulates salt and water balance in the body, thus controlling blood pressure. When the adrenal glands fail to produce adequate amounts of these hormones, Addison's Disease develops.
Causes of Addison's Disease
Addison's Disease can result from various underlying causes, including autoimmune disorders, infections, genetic factors, or damage to the adrenal glands. Here are some common causes:
1. Autoimmune Disorders: In about 70-80% of cases, Addison's Disease occurs due to autoimmune destruction of the adrenal glands. In this scenario, the body's immune system mistakenly attacks and damages the adrenal cortex, leading to decreased hormone production.
2. Infections: Tuberculosis (TB) is a common infectious cause of Addison's Disease, particularly in developing countries. Other infections, such as fungal infections or HIV, can also affect the adrenal glands and lead to adrenal insufficiency.
3. Genetic Factors: Rarely, Addison's Disease can be inherited due to genetic mutations affecting the adrenal glands' function. These genetic conditions may present in childhood or later in life.
4. Surgical Removal or Damage: Surgical removal of the adrenal glands (adrenalectomy) due to conditions like tumors or trauma can result in Addison's Disease if both glands are removed or if the remaining gland is unable to produce enough hormones.
5. Medications: Prolonged use of certain medications, such as corticosteroids, which are commonly prescribed for conditions like asthma, rheumatoid arthritis, or lupus, can suppress the adrenal glands' function, leading to adrenal insufficiency when discontinued abruptly.
Symptoms of Addison's Disease
The symptoms of Addison's Disease can vary widely and may develop gradually over time. Early detection and treatment are crucial to prevent complications. Some common symptoms include:
1. Fatigue and Weakness: Persistent fatigue and weakness, even after adequate rest, are hallmark symptoms of Addison's Disease. Patients often report feeling tired and exhausted, regardless of their activity level.
2. Weight Loss and Decreased Appetite: Unintentional weight loss and loss of appetite are common in individuals with Addison's Disease. Despite eating regularly, patients may struggle to maintain their weight.
3. Low Blood Pressure (Hypotension): Addison's Disease can cause low blood pressure, leading to dizziness, lightheadedness, and fainting spells, especially upon standing up (orthostatic hypotension).
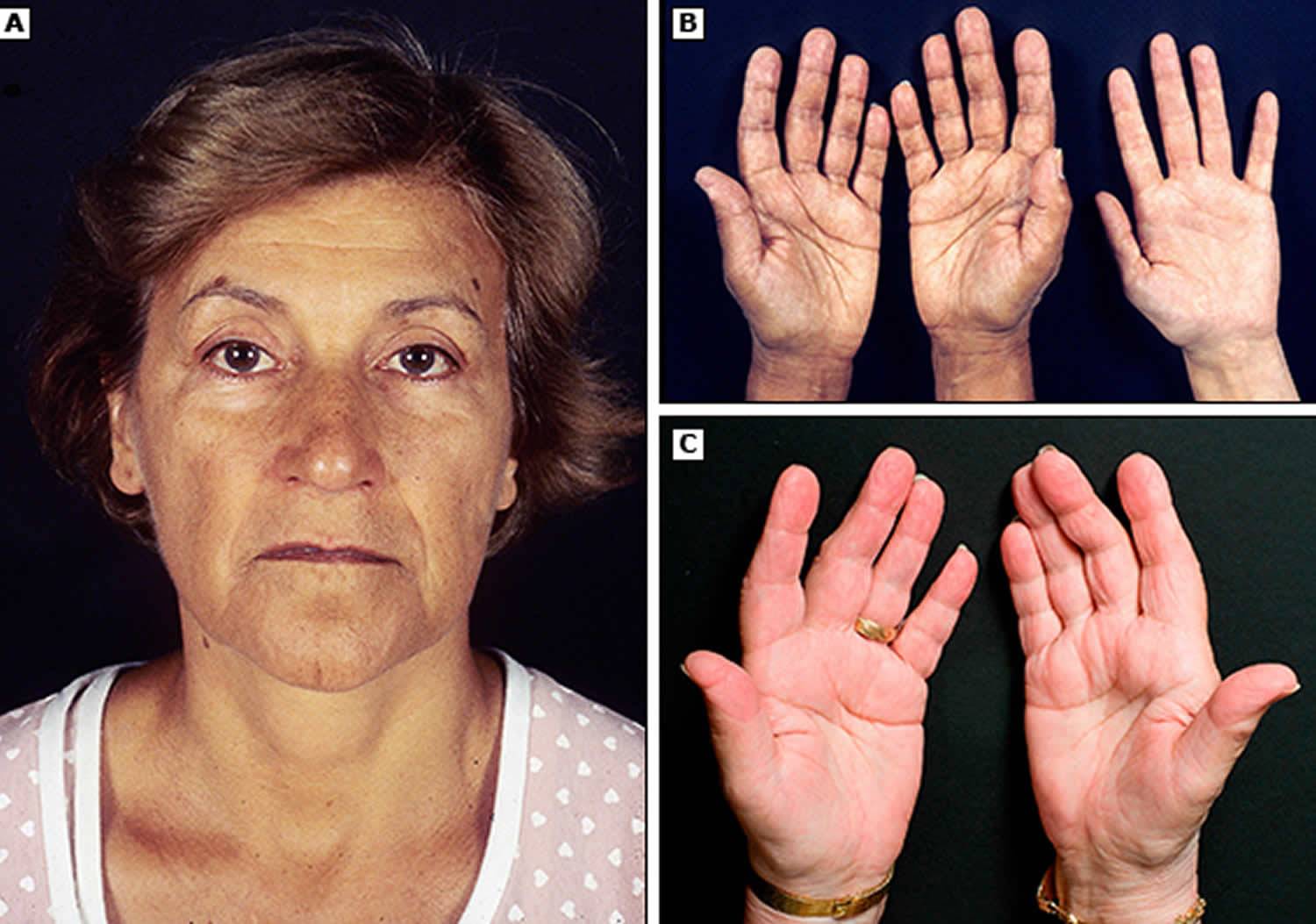
4. Hyperpigmentation: One distinctive feature of Addison's Disease is hyperpigmentation, or darkening of the skin, which typically occurs in sun-exposed areas and skin folds. This is due to increased production of melanin stimulated by elevated levels of adrenocorticotropic hormone (ACTH), which is involved in the regulation of cortisol.
5. Salt Cravings and Low Blood Sugar: As aldosterone levels decrease in Addison's Disease, the body may lose excessive amounts of salt, leading to salt cravings and low sodium levels (hyponatremia). This can cause symptoms like muscle weakness, nausea, and fatigue. Additionally, inadequate cortisol levels can result in low blood sugar (hypoglycemia), leading to symptoms such as shakiness, sweating, and confusion.
6. Gastrointestinal Symptoms: Digestive issues such as nausea, vomiting, diarrhea, and abdominal pain are common in Addison's Disease and may mimic symptoms of other gastrointestinal disorders.
7. Mood Changes and Depression: Changes in mood, irritability, and depression can occur in individuals with Addison's Disease, possibly due to hormonal imbalances and the stress of managing a chronic illness.
Diagnosis of Addison's Disease
Diagnosing Addison's Disease can be challenging due to its nonspecific symptoms, which can overlap with other medical conditions. However, a thorough evaluation by a healthcare professional, including a detailed medical history, physical examination, and specific tests, can help confirm the diagnosis. Here are some common diagnostic tests for Addison's Disease:
1. Blood Tests: Blood tests are used to measure the levels of cortisol, aldosterone, and ACTH in the blood. Low cortisol levels, along with high ACTH levels, are indicative of primary adrenal insufficiency. Sodium, potassium, and glucose levels may also be measured to assess electrolyte imbalances and hypoglycemia.
2. ACTH Stimulation Test: This test involves injecting synthetic ACTH and measuring cortisol levels before and after the injection. In individuals with Addison's Disease, cortisol levels typically remain low even after ACTH stimulation.
3. Imaging Studies: Imaging tests such as CT (computed tomography) or MRI (magnetic resonance imaging) scans may be performed to evaluate the size and structure of the adrenal glands and identify any abnormalities or damage.
4. Antibody Tests: In cases suspected to be autoimmune in nature, antibody tests may be conducted to detect specific antibodies associated with autoimmune adrenal insufficiency, such as anti-adrenal antibodies or anti-21-hydroxylase antibodies.
It's important to note that the diagnosis of Addison's Disease requires careful interpretation of clinical findings and laboratory test results, as well as consideration of other possible causes of adrenal insufficiency.
Treatment of Addison's Disease
Treatment for Addison's Disease involves replacing the deficient hormones to restore hormonal balance and alleviate symptoms. This typically involves lifelong hormone replacement therapy and close monitoring by a healthcare provider. Here are the main components of treatment:
1. Cortisol Replacement: The cornerstone of treatment for Addison's Disease is cortisol replacement therapy with oral glucocorticoids, such as hydrocortisone, prednisone, or dexamethasone. These medications mimic the action of cortisol and help regulate metabolism, inflammation, and the body's response to stress.
2. Aldosterone Replacement: In cases where aldosterone production is also impaired, aldosterone replacement therapy may be necessary. This usually involves taking oral mineralocorticoid medications such as fludrocortisone, which help maintain salt and water balance and prevent electrolyte imbalances.
3. Individualized Dosing: Hormone replacement therapy is typically tailored to each patient based on their symptoms, hormone levels, and response to treatment. The goal is to achieve optimal hormone levels while minimizing side effects and complications.
4. Stress Management:
Individuals with Addison's Disease are at increased risk of adrenal crisis, a life-threatening condition characterized by severe cortisol deficiency. Therefore, it's essential for patients to learn how to manage stress, recognize the signs of adrenal crisis, and take appropriate measures, such as increasing cortisol doses during illness, surgery, or other stressful situations.
5. Dietary Considerations: Maintaining a balanced diet and adequate hydration are important for managing Addison's Disease and preventing complications such as electrolyte imbalances. Patients may need to increase their salt intake, especially during hot weather or periods of heavy sweating.
6. Medication Adjustments: Certain medications, such as corticosteroids, may need to be adjusted or temporarily increased during times of illness or stress to prevent adrenal crisis. Patients should always inform their healthcare providers about their Addison's Disease diagnosis and any medications they are taking.
7. Regular Monitoring: Close monitoring by a healthcare provider is essential to ensure that hormone replacement therapy is effective and to detect any complications or changes in hormone levels. This may involve regular blood tests to assess hormone levels, electrolytes, and other markers of adrenal function.
Living with Addison's Disease
Living with Addison's Disease requires ongoing self-management and vigilance to maintain optimal health and prevent complications. Here are some tips for managing Addison's Disease effectively:
1. Take Medications as Prescribed: It's crucial to take hormone replacement medications exactly as prescribed by a healthcare provider and not to skip doses. Missing doses or abruptly stopping medication can lead to adrenal crisis.
2. Wear Medical Alert Jewelry: Wearing a medical alert bracelet or necklace that indicates you have Addison's Disease can alert healthcare providers in case of an emergency, such as adrenal crisis, when you may be unable to communicate.
3. Carry Emergency Supplies: Keep an emergency kit with extra medication, a steroid injection (such as hydrocortisone or dexamethasone) for adrenal crisis, and instructions on how to administer it in case of emergency.
4. Stay Informed: Educate yourself about Addison's Disease, its symptoms, and treatment options. Be proactive in managing your condition and advocate for yourself with healthcare providers.
5. Communicate with Healthcare Providers: Keep regular follow-up appointments with your healthcare provider and communicate any changes in symptoms or concerns promptly. Working closely with your healthcare team can help optimize treatment and prevent complications.
6. Manage Stress: Practice stress-reduction techniques such as mindfulness, relaxation exercises, or yoga to help manage stress and reduce the risk of adrenal crisis.
7. Stay Hydrated: Drink plenty of fluids, especially in hot weather or during periods of increased physical activity, to prevent dehydration and maintain electrolyte balance.
Conclusion
Addison's Disease is a chronic condition characterized by adrenal insufficiency, resulting from decreased production of cortisol and often aldosterone by the adrenal glands. While relatively rare, it can have serious consequences if left untreated. Early recognition, diagnosis, and appropriate management are essential to prevent complications and maintain a good quality of life for individuals living with Addison's Disease.
By understanding the causes, symptoms, diagnosis, and treatment options for Addison's Disease, healthcare providers and patients alike can work together to effectively manage this condition and minimize its impact on daily life. With proper medical care, lifestyle adjustments, and self-management strategies, individuals with Addison's Disease can lead full and active lives.



No comments yet
Be the first to share your thoughts!