Type 1 Diabetes: Symptoms, Causes, Treatment, and Management
Type 1 diabetes is a chronic autoimmune condition that affects millions of people worldwide. Unlike type 2 diabetes, which is often associated with lifestyle factors, type 1 diabetes typically develops early in life and is not preventable. In this comprehensive guide, we will delve into the intricacies of type 1 diabetes, including its symptoms, causes, treatment options, and strategies for managing this condition effectively.
**1. What is Type 1 Diabetes?**
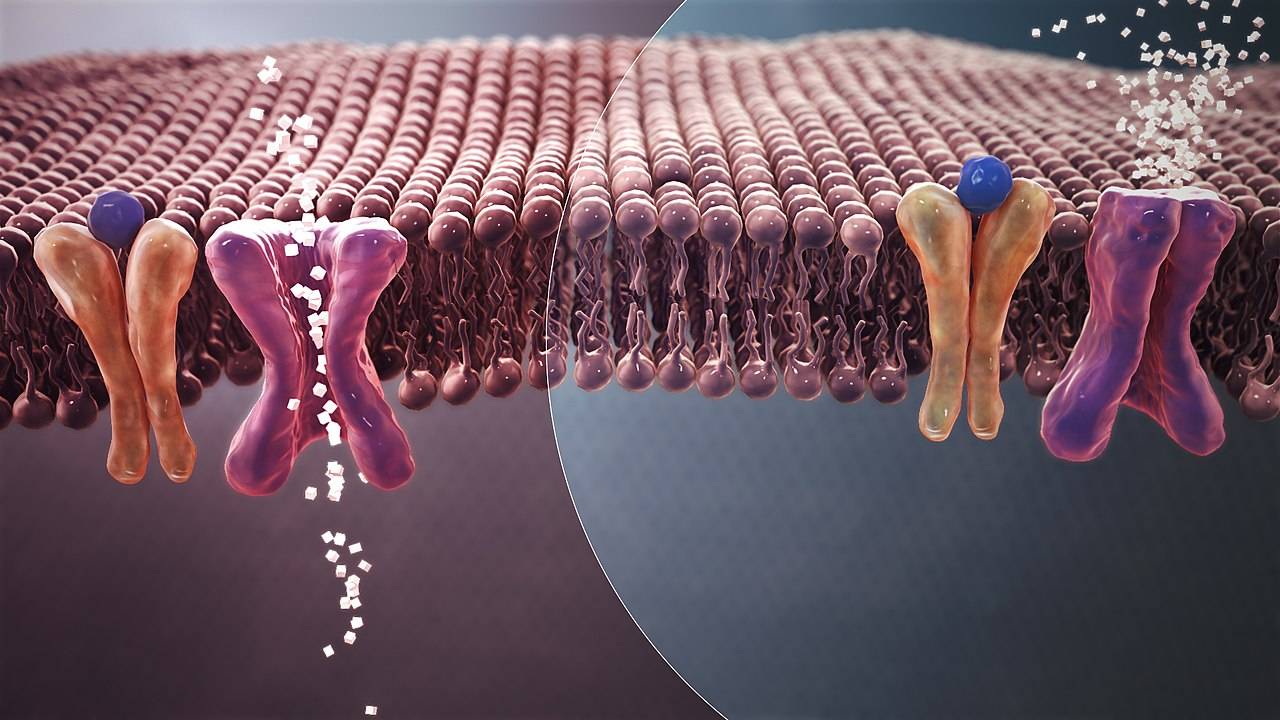
Type 1 diabetes, formerly known as juvenile diabetes or insulin-dependent diabetes, is a condition characterized by the immune system's destruction of insulin-producing beta cells in the pancreas. Insulin is a hormone that regulates blood sugar (glucose) levels by facilitating the uptake of glucose into cells for energy production. Without sufficient insulin, glucose accumulates in the bloodstream, leading to high blood sugar levels, known as hyperglycemia.
**2. Symptoms of Type 1 Diabetes**
The symptoms of type 1 diabetes often develop rapidly and can include:
- Excessive thirst (polydipsia)
- Frequent urination (polyuria)
- Extreme hunger (polyphagia)
- Unexplained weight loss
- Fatigue and weakness
- Blurred vision
- Irritability and mood changes
- Nausea and vomiting
These symptoms may vary in severity and may be accompanied by ketones in the urine, a condition known as diabetic ketoacidosis (DKA). DKA is a life-threatening complication of untreated or inadequately managed type 1 diabetes and requires immediate medical attention.
**3. Causes of Type 1 Diabetes**
The exact cause of type 1 diabetes is not fully understood, but it is believed to involve a combination of genetic, autoimmune, and environmental factors.
**Genetic Factors:** Individuals with a family history of type 1 diabetes are at a higher risk of developing the condition. Certain genes associated with the immune system may predispose individuals to autoimmune reactions against the pancreatic beta cells.
**Autoimmune Response:** Type 1 diabetes is considered an autoimmune disease, meaning the body's immune system mistakenly attacks and destroys its own cells. In the case of type 1 diabetes, immune cells target and destroy the insulin-producing beta cells in the pancreas. The triggering factor for this autoimmune response is not well-defined, but viral infections and other environmental factors have been implicated.
**Environmental Triggers:** Environmental factors, such as viral infections, dietary factors, and exposure to toxins, may trigger the onset of type 1 diabetes in genetically susceptible individuals. Viral infections, particularly those caused by enteroviruses, have been linked to the development of type 1 diabetes by triggering an autoimmune response in genetically predisposed individuals.
**4. Diagnosis of Type 1 Diabetes**
The diagnosis of type 1 diabetes is based on clinical symptoms, blood tests, and other diagnostic criteria. Common tests used to diagnose type 1 diabetes include:
- **Fasting Blood Sugar Test:** Measures blood glucose levels after a period of fasting.
- **Random Blood Sugar Test:** Measures blood glucose levels at any time of the day, regardless of when the individual last ate.
- **Hemoglobin A1c Test:** Provides an estimate of average blood glucose levels over the past two to three months.
- **Glycated Albumin Test:** Measures the percentage of glycated albumin in the blood, providing information about short-term changes in blood glucose levels.
- **Ketone Testing:** Measures the presence of ketones in the urine or blood, indicating the breakdown of fat for energy due to insufficient insulin.
In addition to these tests, healthcare providers may perform antibody tests to detect autoimmune markers associated with type 1 diabetes, such as islet cell antibodies (ICA), insulin autoantibodies (IAA), glutamic acid decarboxylase antibodies (GADA), and zinc transporter 8 antibodies (ZnT8).
**5. Treatment of Type 1 Diabetes**
The primary goal of treating type 1 diabetes is to maintain blood glucose levels within a target range to prevent complications while minimizing the risk of hypoglycemia (low blood sugar). Treatment strategies for type 1 diabetes typically include:
- **Insulin Therapy:** Since individuals with type 1 diabetes produce little to no insulin, exogenous insulin must be administered via injections or an insulin pump. Multiple types of insulin are available, including rapid-acting, short-acting, intermediate-acting, and long-acting formulations, allowing for flexible insulin regimens tailored to individual needs.
- **Blood Glucose Monitoring:** Regular self-monitoring of blood glucose levels is essential for adjusting insulin doses, identifying patterns, and preventing hyperglycemia and hypoglycemia. Continuous glucose monitoring (CGM) systems provide real-time glucose readings and trend data, offering greater insight into blood sugar control.
- **Carbohydrate Counting:** Carbohydrate counting involves estimating the amount of carbohydrates in meals and adjusting insulin doses accordingly to maintain blood glucose levels within target ranges. This approach allows for greater flexibility in meal planning and insulin dosing.
- **Healthy Lifestyle Habits:** Adopting a healthy lifestyle, including regular physical activity, a balanced diet, adequate sleep, stress management, and avoiding tobacco and excessive alcohol consumption, can help improve blood sugar control and reduce the risk of complications.
- **Education and Support:** Diabetes education programs and support groups can provide valuable information, skills, and emotional support for individuals with type 1 diabetes and their families. Learning about diabetes management, self-care practices, problem-solving strategies, and coping mechanisms can empower individuals to take control of their health and well-being.
**6. Complications of Type 1 Diabetes**
Poorly controlled type 1 diabetes can lead to various acute and chronic complications, including:
- **Acute Complications:**
- Diabetic ketoacidosis (DKA)
- Hyperosmolar hyperglycemic state (HHS)
- Hypoglycemia (low blood sugar)
- Hyperglycemic hyperosmolar nonketotic syndrome (HHNS)
- **Chronic Complications:**
- Cardiovascular disease (heart disease, stroke)
- Kidney disease (diabetic nephropathy)
- Nerve damage (diabetic neuropathy)
- Eye damage (diabetic retinopathy)
- Foot damage (diabetic foot ulcers, amputations)
- Skin conditions (bacterial and fungal infections)
Preventing and managing these complications requires comprehensive diabetes care, including regular medical screenings, blood sugar monitoring, medication management, lifestyle modifications, and adherence to treatment regimens.
**7. Research and Innovations in Type 1 Diabetes**
Advances in research and technology continue to revolutionize the management of type 1 diabetes and improve outcomes for individuals living with the condition. Some notable developments include:
- **Artificial Pancreas Systems:** Closed-loop insulin delivery systems, also known as artificial pancreas systems, combine continuous glucose monitoring with automated insulin delivery, mimicking the function of a healthy pancreas. These systems adjust insulin doses in real-time based on glucose readings, reducing the burden of diabetes management and improving blood sugar control.
- **Insulin Delivery Devices:** Innovations in insulin delivery devices, such as insulin pumps, insulin pens, and needle-free injection systems, offer greater convenience, precision, and flexibility in insulin administration, enhancing treatment adherence and quality of life.
- **Islet Cell Transplantation:** Islet cell transplantation involves transplanting insulin-producing
islet cells from donor pancreases into individuals with type 1 diabetes. While still considered an experimental treatment, islet cell transplantation holds promise for restoring insulin independence and improving glycemic control in select patients.
- **Immunotherapy:** Immunotherapy approaches aim to modulate the immune system to prevent or halt the autoimmune destruction of pancreatic beta cells in type 1 diabetes. These strategies may involve immune-modulating medications, vaccines, or interventions to induce immune tolerance and preserve beta cell function.
**8. Living with Type 1 Diabetes**
Living with type 1 diabetes presents unique challenges that require ongoing management, adaptation, and resilience. Some tips for effectively managing type 1 diabetes and optimizing quality of life include:
- **Stay Informed:** Educate yourself about type 1 diabetes, its treatment options, and self-care practices to make informed decisions and take an active role in your health.
- **Monitor Blood Sugar:** Regularly monitor your blood glucose levels and keep track of patterns, trends, and factors that affect your blood sugar control.
- **Follow a Healthy Lifestyle:** Eat a balanced diet, engage in regular physical activity, get adequate sleep, manage stress effectively, and avoid unhealthy habits to promote overall well-being and blood sugar management.
- **Seek Support:** Connect with healthcare providers, diabetes educators, support groups, and peers who understand your experiences and can provide guidance, encouragement, and emotional support.
- **Plan Ahead:** Plan ahead for meals, physical activity, medication management, and emergencies to minimize disruptions and ensure consistent diabetes care.
**Conclusion**
Type 1 diabetes is a complex and challenging condition that requires lifelong management and support. By understanding the symptoms, causes, treatment options, and strategies for managing type 1 diabetes effectively, individuals with the condition can take control of their health, prevent complications, and live full and active lives. With ongoing research, innovation, and advancements in diabetes care, the future holds promise for improved treatments, better outcomes, and ultimately, a cure for type 1 diabetes.



No comments yet
Be the first to share your thoughts!