Preventing Type 1 Diabetes
Type 1 diabetes, often referred to as juvenile diabetes, is a chronic autoimmune condition in which the pancreas produces little to no insulin. Unlike Type 2 diabetes, which is largely preventable through lifestyle changes, Type 1 diabetes is not directly linked to lifestyle factors such as diet and exercise. Instead, it occurs when the body's immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. While the exact cause of Type 1 diabetes remains unknown, several strategies may help reduce the risk of developing this condition. In this comprehensive guide, we will explore various approaches to preventing Type 1 diabetes and managing its risk factors.
Understanding Type 1 Diabetes:
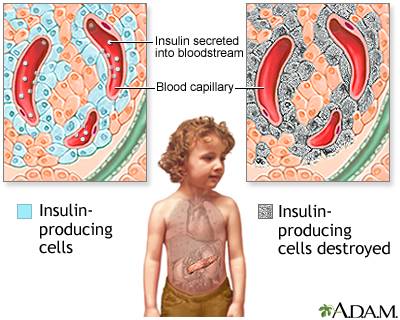
Before delving into prevention strategies, it's essential to have a basic understanding of Type 1 diabetes and its underlying mechanisms. In Type 1 diabetes, the body's immune system targets beta cells in the pancreas, which are responsible for producing insulin. Insulin is a hormone that regulates blood sugar levels by facilitating the uptake of glucose into cells for energy. Without adequate insulin production, glucose accumulates in the bloodstream, leading to high blood sugar levels and various health complications.
Type 1 diabetes typically develops during childhood or adolescence, although it can occur at any age. The exact cause of this autoimmune response is not fully understood, but genetic predisposition and environmental factors are believed to play significant roles. Researchers continue to study the complex interplay between genetics, viral infections, and environmental triggers in the development of Type 1 diabetes.
Prevention Strategies:
While it's not currently possible to prevent Type 1 diabetes entirely, several strategies may help reduce the risk or delay its onset, especially in individuals with a family history of the condition. Here are some key prevention strategies to consider:
1. Genetic Screening:
Genetic screening can help identify individuals who may be at higher risk of developing Type 1 diabetes based on their genetic profile. By analyzing specific genetic markers associated with the condition, healthcare providers can offer personalized risk assessments and guidance for preventive measures.
2. Early Detection:
Early detection of autoimmune markers and beta cell dysfunction can provide valuable insights into the progression of Type 1 diabetes. Regular screening tests, such as autoantibody tests and glucose tolerance tests, can help identify individuals in the early stages of the disease process, allowing for timely intervention and monitoring.
3. Immunomodulatory Therapy:
Immunomodulatory therapies aim to modulate the immune system's response to prevent or slow the destruction of beta cells in the pancreas. These therapies may include immunosuppressive drugs, such as corticosteroids or monoclonal antibodies, which target specific immune cells involved in the autoimmune process. While still experimental, ongoing clinical trials are investigating the efficacy and safety of various immunomodulatory approaches for preventing Type 1 diabetes.
4. Dietary Interventions:
While dietary factors do not directly cause Type 1 diabetes, certain dietary interventions may help modulate the immune system and reduce inflammation, potentially lowering the risk of autoimmune diseases. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins provides essential nutrients and antioxidants that support immune function and overall health. Additionally, breastfeeding during infancy has been associated with a reduced risk of Type 1 diabetes in children with a genetic predisposition to the condition.
5. Vitamin D Supplementation:
Vitamin D plays a crucial role in immune regulation and may influence the risk of autoimmune diseases, including Type 1 diabetes. Studies have suggested an inverse relationship between vitamin D levels and the incidence of Type 1 diabetes, with higher vitamin D levels associated with a lower risk of the condition. While more research is needed to establish a causal relationship, vitamin D supplementation may be beneficial, especially in individuals with vitamin D deficiency or insufficiency.
6. Environmental Factors:
Environmental factors, such as viral infections and exposure to certain toxins, have been implicated in the development of Type 1 diabetes. Minimizing exposure to potential triggers, such as cigarette smoke, chemical pollutants, and viral infections, may help reduce the risk of autoimmune reactions in susceptible individuals. Additionally, promoting a healthy lifestyle that includes regular exercise, stress management, and adequate sleep can support immune function and overall well-being.
7. Participating in Clinical Trials:
Clinical trials play a vital role in advancing our understanding of Type 1 diabetes and developing new preventive strategies and treatments. By participating in clinical trials, individuals at risk of Type 1 diabetes can contribute to research efforts aimed at identifying effective interventions and ultimately preventing the condition in future generations.
Managing Risk Factors:
While it may not be possible to completely eliminate the risk of developing Type 1 diabetes, managing known risk factors can help reduce the likelihood of the condition or its complications. Here are some additional steps individuals can take to manage their risk factors:
1. Regular Monitoring:
Regular monitoring of blood sugar levels, autoimmune markers, and other relevant health parameters can help individuals stay informed about their risk of developing Type 1 diabetes. Working closely with healthcare providers to track changes over time and adjust preventive measures as needed is essential for early detection and intervention.
2. Maintaining a Healthy Weight:
Although obesity is not a risk factor for Type 1 diabetes, maintaining a healthy weight through balanced nutrition and regular exercise is important for overall health and well-being. Obesity is a significant risk factor for Type 2 diabetes and other chronic conditions, so adopting healthy lifestyle habits can help reduce the risk of developing multiple health issues.
3. Blood Sugar Management:
For individuals with Type 1 diabetes or those at risk of developing the condition, maintaining stable blood sugar levels is critical for preventing complications and optimizing long-term health outcomes. This involves monitoring blood sugar regularly, following a personalized meal plan, taking insulin or other prescribed medications as directed, and incorporating physical activity into daily routines.
4. Education and Support:
Education and support are essential components of diabetes prevention and management. Empowering individuals with knowledge about the condition, self-care strategies, and available resources can help them make informed decisions and navigate the challenges of living with or at risk of Type 1 diabetes. Support from healthcare providers, diabetes educators, support groups, and online communities can also provide invaluable guidance and encouragement.
Conclusion:
While Type 1 diabetes cannot be prevented entirely, proactive measures can help reduce the risk or delay its onset in susceptible individuals. By leveraging advances in genetic screening, early detection, immunomodulatory therapy, lifestyle interventions, and ongoing research, we can work towards a future where Type 1 diabetes is more effectively managed and ultimately prevented. Empowering individuals with knowledge, support, and access to resources is essential for promoting optimal health and well-being in the face of this chronic autoimmune condition. Through collaborative efforts across healthcare disciplines, research institutions, and advocacy organizations, we can continue to advance our understanding of Type 1 diabetes and improve outcomes for individuals affected by this condition now and in the future.