Macular Degeneration: Causes, Symptoms, Treatments, and Prevention
Introduction to Macular Degeneration:
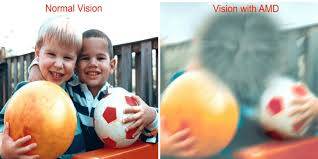
Macular degeneration, often referred to as age-related macular degeneration (AMD), is a progressive eye condition that affects millions of people worldwide, particularly those over the age of 50. It is a leading cause of vision loss among older adults. As life expectancy increases globally, the prevalence of AMD is also expected to rise. Understanding this condition, its causes, symptoms, available treatments, and preventive measures is crucial for both affected individuals and healthcare providers.
In this comprehensive guide, we will delve into the various aspects of macular degeneration, shedding light on its pathology, risk factors, diagnosis, management strategies, and ongoing research efforts aimed at combating this sight-threatening condition.
I. Anatomy and Function of the Macula:
Before delving into the intricacies of macular degeneration, it's essential to understand the anatomy and function of the macula, as it is the primary site affected by this condition.
The macula is a small, specialized area located near the center of the retina, which is the light-sensitive tissue lining the back of the eye. It is responsible for central vision, which allows us to see fine details clearly and perform tasks such as reading, driving, and recognizing faces. The macula contains a high concentration of photoreceptor cells called cones, which are responsible for color vision and detailed central vision.
II. Types of Macular Degeneration:
Macular degeneration can be broadly classified into two main types: dry AMD and wet AMD. Each type has distinct characteristics in terms of progression, symptoms, and management.
1. Dry Macular Degeneration (Non-neovascular AMD):
Dry AMD is the more common form, accounting for approximately 80-90% of all AMD cases. It is characterized by the gradual breakdown or thinning of the macular tissue and the formation of small, yellowish deposits called drusen beneath the retina. These deposits can interfere with the normal function of the macula, leading to central vision loss over time.
Symptoms of dry AMD may include:
- Blurred or distorted central vision
- Difficulty reading or recognizing faces
- Decreased contrast sensitivity
- The appearance of dark spots or visual distortions in the central visual field
2. Wet Macular Degeneration (Neovascular AMD):
Wet AMD, although less common than dry AMD, is responsible for the majority of severe vision loss associated with macular degeneration. It is characterized by the growth of abnormal blood vessels beneath the retina, a process known as choroidal neovascularization (CNV). These fragile vessels can leak fluid and blood into the macula, causing rapid and severe damage to central vision.
Symptoms of wet AMD may include:
- Sudden or rapid loss of central vision
- Distorted or wavy vision
- Visual hallucinations (metamorphopsia)
- A dark spot or blind spot in the central visual field
III. Risk Factors for Macular Degeneration:
While the exact cause of macular degeneration remains unclear, several risk factors have been identified that may increase an individual's likelihood of developing the condition. Understanding these risk factors is crucial for early detection and intervention.
1. Age:
Age is the most significant risk factor for macular degeneration, with the prevalence of the condition increasing with advancing age. Most cases of AMD are diagnosed in individuals over the age of 50, and the risk continues to rise with each decade of life.
2. Genetics:
Genetic factors play a significant role in the development of macular degeneration. Individuals with a family history of AMD are at a higher risk of developing the condition themselves. Several genes have been implicated in the pathogenesis of AMD, including those involved in inflammation, lipid metabolism, and the complement system.
3. Smoking:
Smoking is a well-established modifiable risk factor for macular degeneration. Smokers are at a significantly higher risk of developing both dry and wet AMD compared to non-smokers. The harmful effects of smoking on ocular health are thought to result from oxidative stress, inflammation, and damage to the blood vessels supplying the retina.
4. Race and Ethnicity:
Certain racial and ethnic groups have been found to have a higher prevalence of macular degeneration. Caucasians, particularly those of European descent, are at a greater risk compared to other ethnicities. Additionally, individuals with lighter eye color may be more susceptible to AMD due to lower levels of protective pigmentation in the retina.
5. Cardiovascular Health:
There is growing evidence to suggest that cardiovascular risk factors, such as hypertension, high cholesterol, and obesity, may also influence the development and progression of macular degeneration. These systemic conditions can affect the blood flow to the retina and contribute to the formation of drusen and abnormal blood vessels.
6. Sun Exposure:
Prolonged exposure to ultraviolet (UV) radiation from the sun may increase the risk of developing macular degeneration. UV light can induce oxidative damage to the retinal cells and promote inflammation, which are key processes implicated in the pathogenesis of AMD. Wearing sunglasses with UV protection and avoiding excessive sun exposure may help mitigate this risk.
IV. Diagnosis and Evaluation:
Early diagnosis and prompt intervention are critical for preserving vision in individuals with macular degeneration. Ophthalmologists and optometrists employ various diagnostic tests and imaging modalities to assess the severity of the condition and monitor disease progression.
1. Comprehensive Eye Examination:
A comprehensive eye examination is the first step in diagnosing macular degeneration. This typically includes a visual acuity test to assess central and peripheral vision, a dilated fundus examination to examine the retina and macula, and tonometry to measure intraocular pressure.
2. Amsler Grid Test:
The Amsler grid is a simple tool used to detect central vision abnormalities indicative of macular degeneration. Patients are instructed to focus on a central point while viewing a grid pattern of straight lines. Distortions, wavy lines, or missing areas in the grid may suggest macular pathology and warrant further evaluation.
3. Optical Coherence Tomography (OCT):
OCT is a non-invasive imaging technique that provides high-resolution cross-sectional images of the retina and macula. It allows clinicians to visualize the thickness and integrity of retinal layers, identify the presence of drusen, and detect signs of macular edema or CNV. OCT imaging is invaluable for monitoring disease progression and evaluating treatment response in patients with AMD.
4. Fluorescein Angiography (FA):
Fluorescein angiography is a diagnostic procedure used to assess the retinal vasculature and detect abnormal blood vessel growth in wet AMD. A fluorescent dye is injected into the bloodstream, and sequential photographs are taken as the dye circulates through the retinal vessels. Areas of leakage or blockage of dye may indicate the presence of CNV, guiding treatment decisions.
V. Treatment Options for Macular Degeneration:
While there is currently no cure for macular degeneration, several treatment modalities are available to help manage the condition and preserve remaining vision. The choice of treatment depends on the type and severity of AMD, as well as individual patient factors.
1. Dry AMD:
Treatment options for dry AMD are primarily aimed at slowing disease progression and managing symptoms. Although there is no specific pharmacological therapy approved for dry AMD, several nutritional supplements have been shown to have potential benefits in certain patients.
- AREDS Formulation: The Age-Related Eye Disease Study
(AREDS) found that a combination of high-dose antioxidants (vitamins C and E, beta-carotene) and zinc can reduce the risk of progression to advanced AMD in individuals with intermediate to advanced dry AMD. This formulation, known as the AREDS supplement, is recommended for patients at risk of vision loss due to AMD.
- AREDS2 Formulation: Building upon the findings of the original AREDS study, AREDS2 investigated the role of additional supplements, including lutein, zeaxanthin, and omega-3 fatty acids, in the management of AMD. The AREDS2 formulation, which includes these additional nutrients, may offer further protective effects against disease progression.
- Lifestyle Modifications: Adopting a healthy lifestyle that includes a balanced diet rich in fruits, vegetables, and omega-3 fatty acids, maintaining a normal body weight, and avoiding smoking can help reduce the risk of AMD progression. Regular exercise and routine eye examinations are also recommended to monitor changes in vision and ocular health.
2. Wet AMD:
Wet AMD requires more aggressive management due to the rapid and severe vision loss associated with choroidal neovascularization. Treatment modalities for wet AMD primarily target the abnormal blood vessels and aim to prevent further leakage and damage to the macula.
- Anti-VEGF Therapy: Anti-vascular endothelial growth factor (VEGF) agents have revolutionized the treatment of wet AMD by inhibiting the growth of abnormal blood vessels and reducing vascular permeability. Drugs such as ranibizumab, bevacizumab, and aflibercept are administered via intravitreal injections and can help stabilize or improve vision in many patients.
- Photodynamic Therapy (PDT): Photodynamic therapy involves the selective occlusion of abnormal blood vessels using a combination of a photosensitizing drug (verteporfin) and laser light. While less commonly used today compared to anti-VEGF therapy, PDT may still be considered in certain cases, particularly when anti-VEGF treatment alone is insufficient.
- Corticosteroids: Intravitreal corticosteroid injections, such as triamcinolone acetonide or dexamethasone implants, may be used as adjunctive therapy in select patients with wet AMD, particularly those who do not respond adequately to anti-VEGF agents or have contraindications to anti-VEGF treatment.
VI. Emerging Therapies and Research Advances:
Despite significant advancements in the treatment of macular degeneration, ongoing research efforts continue to explore novel therapeutic approaches and potential targets for intervention. Several promising therapies are currently in development or undergoing clinical trials, with the aim of improving outcomes and expanding treatment options for AMD patients.
1. Gene Therapy:
Gene therapy holds great promise for the treatment of inherited retinal disorders, including certain forms of macular degeneration. By delivering functional copies of defective genes or modulating gene expression using viral vectors or gene-editing technologies such as CRISPR-Cas9, researchers aim to correct underlying genetic defects and preserve vision in affected individuals.
2. Stem Cell Therapy:
Stem cell-based approaches offer the potential to regenerate damaged retinal tissue and restore visual function in patients with advanced AMD. Researchers are investigating the use of various stem cell sources, including embryonic stem cells, induced pluripotent stem cells (iPSCs), and adult stem cells, for retinal repair and replacement.
3. Neuroprotection and Anti-inflammatory Strategies:
In addition to targeting angiogenesis and vascular leakage, researchers are exploring neuroprotective and anti-inflammatory interventions aimed at preserving retinal function and preventing photoreceptor cell death in macular degeneration. Therapeutic agents targeting inflammatory mediators, oxidative stress pathways, and neurotrophic factors show promise in preclinical studies and early-phase clinical trials.
4. Retinal Prostheses and Assistive Technologies:
For patients with advanced AMD and irreversible vision loss, retinal prostheses and assistive technologies offer alternative approaches to restore visual perception and improve quality of life. Retinal implants, such as the Argus II retinal prosthesis system, can bypass damaged photoreceptors and directly stimulate remaining retinal cells, allowing patients to perceive light and shapes.
VII. Lifestyle and Nutritional Recommendations:
In addition to medical and surgical interventions, adopting a healthy lifestyle and incorporating specific dietary nutrients into one's daily regimen may help reduce the risk of macular degeneration and support overall ocular health. Several key nutrients have been identified for their potential protective effects against AMD:
- Antioxidants: Vitamins C and E, along with other antioxidants such as beta-carotene and selenium, help neutralize free radicals and reduce oxidative stress in the retina. Foods rich in antioxidants include citrus fruits, berries, nuts, seeds, and leafy green vegetables.
- Lutein and Zeaxanthin: These carotenoid pigments are concentrated in the macula and play a crucial role in filtering harmful blue light and protecting against oxidative damage. Foods high in lutein and zeaxanthin include spinach, kale, corn, and egg yolks.
- Omega-3 Fatty Acids: Essential fatty acids, particularly EPA and DHA found in cold-water fish like salmon, mackerel, and sardines, have anti-inflammatory properties and may help reduce the risk of AMD progression. Plant-based sources of omega-3s include flaxseeds, chia seeds, and walnuts.
- Zinc and Copper: Zinc is involved in numerous biochemical processes essential for retinal function, while copper helps maintain the balance of zinc in the body. Foods rich in zinc include red meat, poultry, shellfish, and legumes, while copper is found in nuts, seeds, whole grains, and seafood.
- Low-Glycemic Index Foods: A diet rich in low-glycemic index (GI) foods, such as whole grains, legumes, fruits, and vegetables, can help stabilize blood sugar levels and reduce the risk of age-related eye diseases, including AMD.
- Hydration: Adequate hydration is essential for maintaining optimal ocular health and preserving the integrity of the retinal tissues. Drinking plenty of water throughout the day can help prevent dryness and irritation of the eyes, especially in individuals with AMD who may be prone to ocular surface disorders.
VIII. The Importance of Regular Eye Examinations:
Regular eye examinations are crucial for the early detection and management of macular degeneration, as well as other ocular conditions that may impact vision and ocular health. Individuals over the age of 50, particularly those with risk factors for AMD, should undergo comprehensive eye screenings at least once a year to monitor changes in vision and retinal health.
During an eye examination, your eye care provider will assess visual acuity, perform a dilated fundus examination to evaluate the retina and macula, and may recommend additional tests such as OCT imaging or fluorescein angiography if macular pathology is suspected. Early intervention and appropriate treatment can help preserve vision and improve outcomes in patients with macular degeneration.
IX. Conclusion:
Macular degeneration is a prevalent and potentially devastating eye condition that affects millions of individuals worldwide, particularly older adults. While there is currently no cure for AMD, advances in diagnostic techniques and treatment modalities have significantly improved outcomes and quality of life for affected individuals.
Early detection, timely intervention, and proactive management are key to slowing disease progression and preserving remaining vision in patients with macular degeneration. Lifestyle modifications, nutritional supplements, and emerging therapeutic approaches offer hope for continued advancements in the field of retinal care and the
eventual eradication of this sight-threatening condition.
By raising awareness, promoting regular eye examinations, and supporting ongoing research efforts, we can work together to combat macular degeneration and ensure a brighter future for individuals affected by this debilitating disease. Let us strive to protect our vision and cherish the gift of sight for generations to come.



No comments yet
Be the first to share your thoughts!