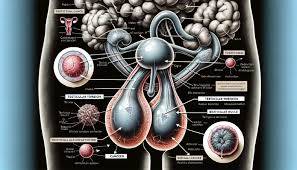
Testicular Atrophy
Testicular atrophy refers to the shrinkage or reduction in the size of one or both testicles, often resulting in impaired function, including reduced testosterone production or sperm output. It can affect fertility and hormonal balance.
---
Causes
Testicular atrophy can result from various factors, including:
1. Infections:
Mumps orchitis or sexually transmitted infections (STIs) like gonorrhea and chlamydia.
2. Hormonal Imbalances:
Low testosterone levels or disturbances in the hypothalamic-pituitary-testicular axis.
Use of anabolic steroids or testosterone supplements.
3. Injury or Trauma:
Physical damage to the testicles leading to loss of tissue.
4. Varicocele:
Enlarged veins in the scrotum can impair blood flow and cause shrinkage over time.
5. Torsion:
Twisting of the spermatic cord cuts off blood supply, leading to tissue death if untreated.
6. Chronic Diseases:
Conditions like liver disease, kidney failure, or diabetes can contribute to atrophy.
7. Radiation or Chemotherapy:
Treatments for cancer may damage testicular tissue.
8. Lifestyle Factors:
Alcohol abuse, drug use (e.g., opioids), and malnutrition.
9. Aging:
Natural decline in testicular size and function with age.
---
Signs and Symptoms
1. Reduction in Testicle Size:
Noticeable shrinkage of one or both testicles.
2. Low Libido and Erectile Dysfunction:
Due to reduced testosterone production.
3. Infertility:
Decreased sperm production or quality.
4. Testicular Pain or Discomfort:
May occur if caused by an underlying condition like infection or torsion.
5. Lack of Secondary Sexual Characteristics:
Reduced muscle mass, body hair, or voice deepness in severe cases.
6. Psychological Symptoms:
Depression, anxiety, or reduced self-esteem related to hormonal changes.
---
Effects
1. Infertility:
Reduced sperm production or motility may impair fertility.
2. Hormonal Deficiency:
Low testosterone levels can affect physical, sexual, and mental health.
3. Chronic Pain:
Persistent pain due to underlying conditions like varicocele or infection.
4. Psychological Impact:
Emotional distress, body image issues, or anxiety over reproductive health.
---
Solutions
1. Diagnosis:
Physical Exam: Assessing size, shape, and consistency of testicles.
Ultrasound: To evaluate blood flow and detect structural abnormalities.
Hormonal Tests: Measuring testosterone, FSH, and LH levels.
Semen Analysis: To assess fertility status.
2. Treat Underlying Causes:
Infections: Antibiotics or antiviral medications for conditions like orchitis or STIs.
Varicocele: Surgical correction (varicocelectomy) to restore blood flow.
Testicular Torsion: Emergency surgery to untwist the spermatic cord.
Hormonal Therapy: Treat hormonal imbalances with testosterone replacement therapy (if appropriate).
3. Lifestyle Modifications:
Maintain a healthy diet and exercise regimen.
Avoid alcohol, recreational drugs, and anabolic steroids.
4. Fertility Preservation:
Sperm Banking: For men planning cancer treatments or at risk of infertility.
Assisted reproductive technologies like IVF may help in severe cases.
5. Supportive Measures:
Counseling or psychological support for coping with the effects of atrophy.
---
Prevention
Protect the testicles during sports or high-risk activities using appropriate gear.
Seek prompt treatment for infections, testicular injuries, or torsion.
Avoid prolonged use of anabolic steroids or unnecessary testosterone supplementation.
Manage chronic conditions like diabetes and varicocele.
---
Prognosis
The outlook for testicular atrophy depends on the underlying cause. Early diagnosis and treatment of reversible causes, such as infections or hormonal imbalances, can restore function. In cases where atrophy is permanent, fertility and hormonal treatments can help mitigate the effects. If you notice testicular changes, consult a healthcare provider for timely intervention.

No comments yet
Be the first to share your thoughts!